Curriculum / Rotations
We offer three tracks (one position each):
- Adult/ Behavioral Medicine (APPIC Code #163913)
- Neuropsychology (APPIC Code #163914)
- Child/Pediatric Psychology (APPIC Code #TBD; New track for 2023-2024 training year)
Each track is organized around training experiences through the Major Rotations. Minor rotations are also required and are designed to complement the skills learned in the major rotations and to round out the trainee’s clinical experiences. We offer the ability to create an individual training plan based on selection of Minor Experiences. Interns will not complete minor experiences that duplicate experiences in their major area.
See links for descriptions:
Behavioral Medicine Major Rotations
Child Track Major Rotations
Neuropsychology Major Rotations
Behavioral Medicine Major Rotations
Throughout the 12 months, the intern spends approximately 3 days per week participating in the experiences below. Interns complete four 6-month rotations (2 rotations are concurrent, 1.5 days each).
Behavioral Medicine Adult/ Young Adult Outpatient Psychology
Supervisors: Stephanie Cox, PhD, ABPP; Colleen Lillard, PhD; Laura Aylward, PhD; or Angelo Giolzetti, PsyD
Location: Chestnut Ridge Center
Interns provide assessment and evidence-based treatment to patients across the life-span with a wide range of presenting problems including those with co-morbid medical and psychiatric concerns. Interns will have regularly scheduled intakes and new patient evaluations throughout the rotation. Interns are encouraged to have a mixture of both short-term and long-term therapy cases. Interns receive supervision primarily from a Cognitive- Behavioral orientation, although interns may also receive training in other evidence-based approaches such as Acceptance and Commitment Therapy and Motivational Interviewing. We are able to select specific patient populations or disorders of interest in order to advance an intern’s training in a specific area or to address any gaps in training.
Pediatric and AYA (adolescent/young adult) Behavioral Medicine/ Psychology Clinic:
Supervisors: Jennifer Ludrosky, PhD; Stephany Lora, PsyD; Jonathan Perle, PhD, ABPP; Janelle Mentrikoski, PhD
Location: Chestnut Ridge Center
Interns will have the option to participate in fully integrated pediatric clinic(s), child/adolescent psychiatric consultation and liaison. Options include:
Pediatric GI Clinic: Interns will attend a half-day pediatric GI clinic (ages 0-18) in order to provide assessment, team consultation, and brief intervention for children and adolescents who present to Gastroenterology. Intervention areas frequently include anxiety, functional abdominal pain, adherence, adjustment to diagnosis, dietary change, encopresis.
Pediatric Nephrology Clinic: Interns will attend a half-day pediatric Nephrology clinic (ages 0-21) in order to provide assessment, team consultation, and brief intervention to children and adolescents who present to Nephrology. Intervention areas include adjustment to diagnosis, complex dietary change, adherence. Interns will practice using MI and stages of change with complex medical patients. Interns will also have the opportunity to join research projects, including examining the link between hypertension and anger in children, and the impact of COVID-19 on blood pressure in children and adolescents.
Pediatric Cleft Palate Clinic: Interns will attend a half-day pediatric Cleft Palate clinic (ages 0- 21) in order to provide psychology assessment and intervention to every clinic patient. Interns will become familiar with important concepts in the treatment of Cleft Lip and Palate and will work closely with large multidisciplinary team to provide high level care for children. Interns will also have the opportunity to gain skills in procedure management, as patients frequently have to undergo in-office procedures.
Parent Management Training (PMT) Clinic: Interns will attend a half-day pediatric clinic (predominantly ages 2-10, but opportunities for older children) where they will learn to (1) provide brief diagnostic assessment of ADHD/disruptive behavior and comorbid challenges, as well as (2) how to implement parent management training strategies; one of the most effective evidence-based interventions for childhood disruptive behavior that is designed to improve compliance, on-task behavior, and parent-child relationships, while reducing problematic behaviors such as defiance and aggression.
ADHD Assessment Clinic: Interns will attend a half-day pediatric clinic (ages 4-11) where they will learn how to conduct in-depth evaluations to determine the presence of ADHD and comorbid psychiatric challenges. Interns will conduct assessment procedures (e.g., interviews, observations, questionnaires), create diagnostic reports, and provide feedback/recommendations.
Attention Deficit/Behavior Clinic (AD/BC): Interns will attend a half-day pediatric clinic (ages 2-10) where they will learn to (1) provide diagnostic assessment of ADHD/disruptive behavior and comorbid challenges, as well as (2) how to implement parent management training strategies; one of the most effective evidence-based interventions for childhood disruptive behavior that is designed to improve compliance, on-task behavior, and parent-child relationships, while reducing problematic behaviors such as defiance and aggression.
Outpatient Pediatric Clinic: The intern will receive training in the provision of outpatient psychological treatment with children, adolescents, and parents. Cognitive Behavioral Therapy, play therapy techniques, and family systems and biopsychosocial theories will be utilized with patients with a variety of ages and presenting problems. Clinic can be focused on specific populations.
AYA (adolescent/young adult) Coping with Chronic Illness Clinic: The intern will participate in outpatient psychotherapy with adolescents and young adults who are living with a variety of chronic illness (e.g. diabetes). Interns will provide CBT focused therapy to help address issues common to this population, including treatment adherence, identity development, and transfer of care.
Supervisors: Stephanie Cox, PhD, ABPP, or Laura Aylward, PhD
Location: Chestnut Ridge Center/ Department of Surgery
WVU Bariatrics offers a comprehensive surgical weight loss program including bariatric- trained surgeons, mid-level providers, dieticians, and psychologists. The intern has the opportunity to work as part of this multidisciplinary team in both assessment and intervention capacities. Interns receive training in pre-surgical psychological evaluations to determine a patient’s appropriateness for surgery. Additionally, interns can provide treatment to patients both pre and post surgically. Concerns commonly addressed include engagement in behavioral changes, treatment of disordered eating behavior, stabilization of psychiatric symptoms, etc. The intern also has the opportunity to attend team case review meetings and observe surgical procedures. The intern will also have the opportunity to lead and/or co-lead a monthly support group for pre- and postoperative patients.
Primary Care Behavioral Health
Supervisors: Barbara Cubic, PhD
Location: Clark K. Sleeth Family Medicine
The goal of this rotation is to increase the intern’s proficiency within the primary-care model; this includes the provision of population-based goal-oriented short-term treatment. The intern will participate in a variety of integrated primary care experiences including:
Integrated Outpatient Clinic:Behavioral health care is integrated into our primary care clinics within the patient-centered medical home model. Common presenting problems in this setting may include comorbid medical/ psychological concerns, insomnia, medication compliance, adjustment disorders, insomnia, relationship stressors, depression/ anxiety.
Family Medicine Inpatient Rounds/ Consultation: Family Medicine patients can continue to receive care by their primary care providers when they are admitted to Ruby Memorial Hospital. The intern has the opportunity to participate as a member of this multidisciplinary inpatient team (alongside residents, medical students, pharmacy, social work, etc.), providing consultation regarding psychological concerns and/or delivering brief psychological interventions in an inpatient setting.
Family Medicine Specialty Clinics: The Department of Family Medicine offers several clinics to provide patients with specialty care to address their specific need. These clinics include the Medical Weight Management Clinic, Diabetes Clinic, and COPD clinic (depending on availability/scheduling). The intern, as a member of these multidisciplinary teams, provides education and treatment of patients’ conditions, including management of psychosocial issues that often co-occur with chronic illnesses. The goal of this team approach is to improve patient outcomes and increase adherence to prescribed treatment regimens. The intern provides consultation and brief assessment or intervention as needed.
Supervision: Interns will meet with each of their supervisors for a total of 2 or more hours per week of individual supervision. Additionally, interns receive informal supervision in the course of observing therapy or conducting co-therapy with the supervisor, staffing after intake evaluations, and in multidisciplinary meetings. Supervision totals 4 or more hours per week.
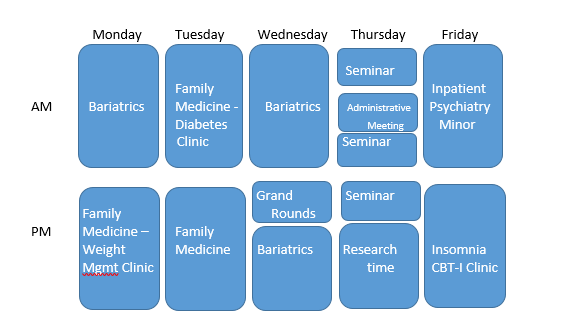
Sample Schedule:
Child Track Major Rotations
Throughout the 12 months, the intern spends approximately 3 days per week participating in the experiences below. Interns complete four 6-month rotations (2 rotations are concurrent, 1.5 days each).
Pediatric Psychology Subspecialty Clinics:
Supervisors: Jennifer Ludrosky, PhD; Stephany Lora, PsyD; Jonathan Perle, PhD, ABPP; Janelle Mentrikoski, PhD
Location: WVU Children’s Hospital
Interns will have the option to participate in fully integrated pediatric clinic(s) and child/adolescent psychiatric consultation and liaison. Options include:
Pediatric GI Clinic: Interns will attend a half-day pediatric GI clinic (ages 0-18) in order to provide assessment, team consultation, and brief intervention for children and adolescents who present to Gastroenterology. Intervention areas frequently include anxiety, functional abdominal pain, adherence, adjustment to diagnosis, dietary change, encopresis.
Pediatric Nephrology Clinic: Interns will attend a half-day pediatric Nephrology clinic (ages 0-21) in order to provide assessment, team consultation, and brief intervention to children and adolescents who present to Nephrology. Intervention areas include adjustment to diagnosis, complex dietary change, adherence. Interns will practice using MI and stages of change with complex medical patients. Interns will also have the opportunity to join research projects, including examining the link between hypertension and anger in children, and the impact of COVID-19 on blood pressure in children and adolescents.
Pediatric Cleft Palate Clinic: Interns will attend a half-day pediatric Cleft Palate clinic (ages 0- 21) in order to provide psychology assessment and intervention to every clinic patient. Interns will become familiar with important concepts in the treatment of Cleft Lip and Palate and will work closely with large multidisciplinary team to provide high level care for children. Interns will also have the opportunity to gain skills in procedure management, supporting children and families during in-office procedures.
Pediatric Cystic Fibrosis Clinic: Interns will attend a half-day pediatric Cystic Fibrosis (CF) clinic (ages 0-21) to provide assessment and brief interventions to every clinic patient. Interns will consult and collaborate with a large multidisciplinary team, including respiratory therapy, social work, dieticians, pharmacy, physical therapy, and physicians. Targeted areas of intervention include adherence to treatment regimens, adjustment to chronic illness, and emotional and behavioral concerns impacting care.
Pediatric Endocrinology Clinic: Interns will attend a half-day pediatric Endocrinology clinic (ages 0-18) to provide assessment and brief interventions with patients who are diagnosed with diabetes. Interns will consult and collaborate with a multidisciplinary team. Targeted areas of intervention include adherence to treatment regimens, adjustment to chronic illness, and emotional and behavioral concerns impacting care.
Family Weight Management Clinic: Interns will attend a half-day family-focused clinic focused on providing behavioral support to families desiring change in health-related behaviors. Interns will have the opportunity to complete intake and follow up visits with children and families, observe specialty physician and dietician visits, and take part in team planning for patient care.
Child and Adolescent Outpatient Psychology/Psychiatry
Supervisors: Jennifer Ludrosky, PhD; Stephany Lora, PsyD; Jonathan Perle, PhD, ABPP, Janelle Mentrikoski, PhD
Location: Chestnut Ridge Center
Outpatient Clinic: Interns provide assessment and evidence-based treatment to children, adolescents, and families with a wide range of presenting problems including those with co-morbid medical and psychiatric concerns. Interns will have regularly scheduled intakes and new patient evaluations throughout the rotation. Interns are encouraged to have a mixture of both short-term and long-term therapy cases. Interns receive supervision primarily from a Cognitive-Behavioral orientation, although interns may also receive training in other evidence-based approaches such as Acceptance and Commitment Therapy, Family Systems, and Motivational Interviewing. We are able to select specific patient populations or disorders of interest in order to advance an intern’s training in a specific area or to address any gaps in training.
Parent Management Training (PMT) Clinic: Interns will attend a half-day pediatric clinic (predominantly ages 2-10, but opportunities for older children) where they will learn to (1) provide brief diagnostic assessment of ADHD/disruptive behavior and comorbid challenges, as well as (2) how to implement parent management training strategies; one of the most effective evidence-based interventions for childhood disruptive behavior that is designed to improve compliance, on-task behavior, and parent-child relationships, while reducing problematic behaviors such as defiance and aggression.
ADHD Assessment Clinic: Interns will attend a half-day pediatric clinic (ages 4-11) where they will learn how to conduct in-depth evaluations to determine the presence of ADHD and comorbid psychiatric challenges. Interns will conduct assessment procedures (e.g., interviews, observations, questionnaires), create diagnostic reports, and provide feedback/recommendations.
Neurodevelopment – Assessment
Supervisors: Jenna Wallace, PsyD; Claire Baniak, PsyD; Krestin Radonovich, PhD
Location: WVU Medicine Children’s Neurodevelopmental Center
Interns on this rotation will provide assessment to children ages 0-12 for a broad variety of presenting neurodevelopmental and early childhood concerns. Interns will operate within the neurodevelopmental team, which is comprised of pediatric psychology and pediatric neurology (with neurodevelopmental specialty, NDD) to provide comprehensive evaluations and care for patients.
Neurodevelopment – Intervention
Supervisors: Claire Baniak, PsyD; Jenna Wallace, PsyD
Location: WVU Medicine Children’s Neurodevelopmental Center
Interns on this rotation will provide evidence based individual and group therapy to children ages 0-12 with neurodevelopmental disabilities. Interns will have regularly scheduled intakes and new patient evaluations throughout the rotation. Interns are encouraged to have a mixture of both short-term and long-term therapy cases. Interns receive supervision primarily from Cognitive-Behavioral and Behavioral orientations. We are able to select specific patient populations or disorders of interest in order to advance an intern’s training in a specific area or to address any gaps in training.
Supervision:
Interns will meet with each of their supervisors for a total of 2 or more hours per week of individual supervision. Additionally, interns receive informal supervision in the course of observing therapy or conducting co-therapy with the supervisor, staffing after intake evaluations, and in multidisciplinary meetings. Supervision totals 4 or more hours per week.
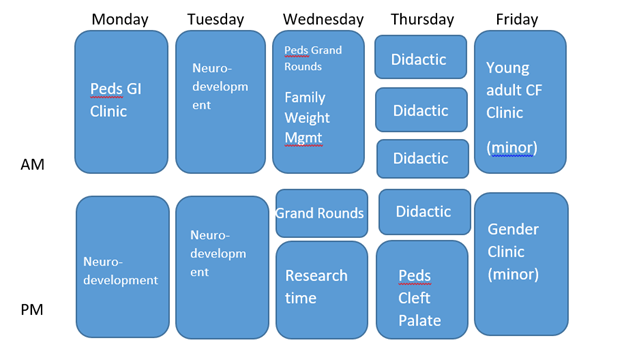
Sample Schedule:
Neuropsychology Major Rotations
The West Virginia University School of Medicine provides a 50% neuropsychology internship training program that is in accordance with the Houston Conference Guidelines. Throughout the 12 months, the intern will complete three, 4-month rotations, working directly with one faculty supervisor for each of the four-month periods. Interns conduct two neuropsychological evaluations per week and participate in feedbacks, psychotherapy, and at times cognitive rehabilitation. The intern participates and gets exposure to awake craniotomy language mapping, Wada evaluations, observation of various neurosurgeries, and participation in several multidisciplinary teams. Interns will participate in weekly neuropsychology-focused case conference, multidisciplinary team meetings, and professional development and Board exam preparation activities. A pediatric neuropsychology rotation is available for the training year.
Major Rotations
The intern will work with three supervisors
Supervisors:
- James J. Mahoney, PhD.
- Liv E. Miller, PsyD, ABPP-CN
- Cierra M. Keith, PhD
- David Scarisbrick, PhD
- Nicholas Jasinski, PhD, ABPP-CN/FR
- Krestin Radonovich, PhD – Pediatric Neuropsychology
- Alexandria Perle, PsyD
All three rotations will focus on the evaluation of primarily outpatients with neurological, medical and psychiatric diseases. Some evaluations are also performed with inpatients in the psychiatric hospital and occasionally in consultation to various services in Ruby Memorial Hospital.
Our clinic offers experience with a rich and diverse patient population, including, but not limited to, individuals with various neurodegenerative conditions, traumatic brain injuries, brain tumors, strokes, movement disorders, cardiovascular disease, learning and attention disorders, and patients diagnosed with severe mental illness and substance abuse. Exposure to neuroimaging is an integral part of the rotation, and patients' MRI, CT, and/or PET scan images are routinely reviewed during evaluations and in didactics. Experiences are also available to interns through the epilepsy surgery program including performing pre- and post-surgical neuropsychological evaluations, attending multidisciplinary treatment team meetings, and participating in Wada evaluations. Pre- and post-surgical DBS evaluations of patients with Parkinson's disease and essential tremor are also frequently performed. In addition, interns may have the opportunity to observe patient rounds, bedside evaluations, neurobehavioral evaluations in multidisciplinary clinics, and provide cognitive rehabilitation with select patients. Finally, the breadth and depth of clinical experiences is enhanced by weekly didactics including Neuropsychology Case Conference including boards preparation, Neurology Grand Rounds, Psychiatry Grand Rounds, Neuromodulation Team meetings, Epilepsy Boards, Brain Tumor Boards, and infrequent observation of brain dissections.
The pediatric neuropsychology rotation includes evaluation of children ages 3 to 16 with complex medical conditions. Referrals include, but are not limited to brain injury, epilepsy, cancer, and neurodevelopmental disorders. Available pediatric didactics include conferences and grand rounds in epilepsy clinic, craniofacial team, neurology, and the neurodevelopmental center.
Supervision: Interns will meet with each of their supervisors for a total of 2 or more hours per week of individual supervision. Additionally, interns receive informal supervision in the course of observing therapy or conducting co-therapy with the supervisor, staffing after intake evaluations, and in multidisciplinary meetings. Supervision occurs prior to the arrival of a patient, during which time records are reviewed and an assessment strategy is planned. Supervision also occurs during the assessment day to address problems or questions as they are encountered and adjust to the assessment accordingly. Supervision totals 4 or more hours per week.
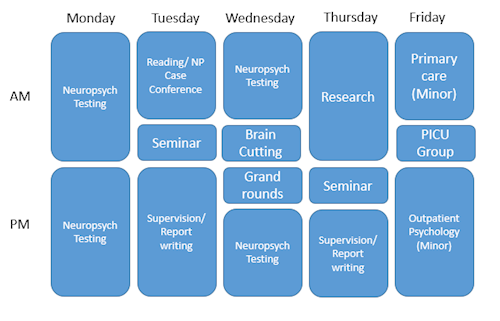
Sample Schedule:
Minor Rotations (Available for Either Track)
Child and Families Multidisciplinary Training Clinic
Supervisor: Jennifer Ludrosky, PhD
Location: Chestnut Ridge Center
The intern will participate in the MDT clinic, which is a team-based, observational and experiential treatment clinic for treating complex children and families. The MDT clinic offers opportunities to work in a team setting with psychiatrists, social workers, psychologists and practicum students from all three disciplines. MDT trainees work under direct observation through the one-way mirror and have the opportunity to observe faculty and other trainees conducting individual and family therapy as well. MDT clinic services highly complex, multi-problem families from CBT and family systems frameworks. The MDT clinic also partners with the WVU Medical Legal clinic, offering interns the opportunity to observe and consult with law students and professors regarding the intersection between medical needs and legal issues.
Forensic Psychology
Supervisor: Colleen Lillard, PhD; Nicholas Jasinski, PhD
Location: Chestnut Ridge Center
The goal of this rotation is to provide interns with an introduction to forensic psychology. At WVU, the forensic section primarily conducts court-ordered evaluations in the following areas: competency to stand trial, criminal responsibility (NGRI), dangerousness, sex offender risk assessment, and fitness for duty. Interns will also be provided didactics in many areas of forensic psychology. This experience is an excellent opportunity for interns from both tracks to learn more about the role a psychologist conducting forensic evaluations and strengthen assessment skills. Additionally, this rotation exposes interns to the state hospital system and strengthens diagnostic and assessment skills working with individuals who have severe mental illnesses.
Behavioral Sleep Medicine
Supervisors: Amy Fiske, PhD
Location: Quinn Curtis Center
This 12-month rotation offers the opportunity for the intern to become proficient in Cognitive-Behavioral Therapy for Insomnia (CBT-I). Additionally, this team is organized as a vertical model of training, in which the intern provides supervision/ oversight for WVU Clinical Psychology graduate students, and also receives training regarding their own supervision skills (“supervision of supervision”).
Concussion Clinic
Supervisor: Nathan Ernst, PsyD
Location: Rockefeller Neuroscience Institute
Interns have the opportunity to participate in acute, subacute, and chronic evaluation and management of sport related concussion and non-athletic trauma. Interns will gain exposure to brief computerized neurocognitive testing (ImPACT), return-to-play management, and lifespan concussion management directed by neuropsychology. Interns will become familiar with targeted, active rehabilitation model for concussion management and will gain exposure to additional team members including athletic trainers, physical therapists, and physicians.
Hospital-Based Psychiatry Consultation and Liaison (General Clinical Team)
Supervisors: Psychiatry attending
Location: Chestnut Ridge Center/Ruby Memorial Hospital
The Psychiatry consultation and liaison team assists in diagnosis and treatment of psychiatric disorders in medically ill patients, who are currently admitted to the hospital. This rotation is an excellent opportunity to increase the intern’s knowledge of psychosomatic medicine and assist in the management of psychiatric disorders within the hospital setting.
Hospital-Based Psychiatry Consultation and Liaison (Substance Use Disorder Team)
Supervisors: Psychiatry attending
Location: Chestnut Ridge Center/Ruby Memorial Hospital
The Psychiatry Consultation and Liaison/ Substance Use Disorder team assists in diagnosis and treatment of substance use disorders in medically ill patients, who are currently admitted to the hospital. More specifically, the intern functions as a member of the multidisciplinary team in providing substance use treatment programing to patients hospitalized with injection drug use-associated infective endocarditis along with other medical conditions.
Outpatient Substance Use Disorders- COAT Program/ MAT Program
Supervisors: Psychiatry Attending
Location: Chestnut Ridge Center
The intern participates in an our intensive outpatient treatment program for Opioid Use Disorders including our Comprehensive Opioid Addiction Treatment (COAT) Program and Medication Assisted Treatment (MAT) Program. These treatment programs include the provision of group medical visits/ medical management for substance use disorders in combination with group therapy sessions. This program is an innovative and successful approach to recovery which has been nationally recognized. The intern participates in observation of group medical visits and can assist in co-leading/ leading groups related to life enrichment skills, relapse prevention, communication skills, and self-esteem skills help individuals get back on track to a healthy, fulfilling life. Groups include Beginners, Intermediate, Advanced recovery group as well as a group for expecting mothers addressing the special clinical needs of women who are pregnant.
Inpatient Substance Use Disorders- Dual Diagnosis Unit
Supervisors: Psychiatry Attending
Location: Chestnut Ridge Center
The intern participates in treatment team rounds on the Dual Diagnosis Unit, a 12-bed inpatient unit for patients who require inpatient detoxification from drugs or alcohol. Interns also have the opportunity to provide psychoeducation and brief treatments to patients while they are hospitalized, which may include teaching relaxation/stress management techniques, relapse prevention skills, and providing assistance with discharge/outpatient treatment planning.
VA Medical Center-Home-Based Primary Care
Supervisor: Rebecca Burnheimer, PhD
Location: Louis A. Johnson VA Medical Center, Clarksburg WV
Interns will have the opportunity to observe home visits with older adult veterans, increase knowledge related to geropsychology, attend interdisciplinary team meetings, and learn more about the role of a psychologist within the Home-Based Primary Care team. This experience is provided at an exposure/ shadowing level for one month or the intern can participate in experiences as they come available.
VA Medical Center-Mental Health Residential Rehabilitation Treatment Program
Supervisors: Amanda Charlton-Fryer, PsyD; Emma Cogar, PsyD
Location: Louis A. Johnson VA Medical Center, Clarksburg WV
Programs: Mental Health Residential Rehabilitation Treatment Program (MH RRTP)
Interns have the opportunity to gain experience in residential treatment of PTSD, substance use disorders, or depression. Interns will provide individual and group psychotherapy, consultation, assessment, treatment planning, and crisis evaluations. Interns will have the opportunity to co-lead and lead groups on topics such as coping skills and cognitive restructuring. Interns will also have the opportunity to learn various evidence-based psychotherapies. In addition, interns will be involved in interdisciplinary morning rounds.
Expanded Research Minor
Supervisors: Research Mentor or Psychology Faculty Member
Location: Chestnut Ridge Center
In addition to the longitudinal research minor (1/2 day per week throughout the year), interns may have the option to devote additional time to research in the 3rd or 4th quarter in order to expand their development in this area. Interns may be allocated an additional ½ day for 3 months in order to expand upon an existing project or develop additional skills. Participation in an expanded research minor is contingent upon the intern demonstrating intermediate to advanced competency in other domains (as evidenced by the Clinical Competency Evaluation and Quarterly Evaluations) and completion of dissertation prior to January 1 of the training year.
Additional Minors for the Adult/ Behavioral Medicine Intern:
Neuropsychology
Supervisors: Liv Miller, PsyD, ABPP-CN; James Mahoney, PhD; David Scarisbrick, PhD; Cierra Keith, PhD; Nicholas Jasinski, PhD, ABPP-CN/FD; Alexandria Perle, PsyD
Location: Chestnut Ridge Center
Interns can receive training in neuropsychological assessment of adult patients with a wide variety of neurological and psychological disorders. The rotation is available at either an introductory or advanced level depending on the intern’s level of experience. The intern can also participate in didactics/ seminars specific to neuropsychology.
Additional Minors for the Neuropsychology Intern:
Pediatric Assessment/ Supervision Training
Supervisor: Jenna Wallace, PsyD; Claire Baniak, PsyD
Location: Neurodevelopment Center
Interns have the opportunity to provide supervision of Clinical Ph.D. graduate students in psychological assessment (IQ, Achievement, executive functioning, and language, with exposure to Autism Spectrum Disorder) in pediatric population (ages 5-12). Interns will gain exposure to various neurodevelopmental disabilities and have the opportunity to interact with various providers involved in assessment cases, such as pediatric neurology, speech language pathology, physical therapy, occupational therapy.
The Neuropsychology intern has the option to participate in any of the Adult Rotations as a Minor experience. See descriptions above in the Behavioral Medicine Track:
Behavioral Medicine Adult/ Young Adult Outpatient Psychology
Supervisors: Stephanie Cox, PhD, ABPP; Colleen Lillard, PhD; Jennifer Ludrosky, PhD; Laura Aylward, PhD; or Angelo Giolzetti, PsyD
Location: Chestnut Ridge Center
Interns provide assessment and evidence-based treatment to patients across the life-span with a wide range of presenting problems including those with co-morbid medical and psychiatric concerns. Interns will have regularly scheduled intakes and new patient evaluations throughout the rotation. Interns are encouraged to have a mixture of both short-term and long-term therapy cases. Interns receive supervision primarily from a Cognitive- Behavioral orientation, although interns may also receive training in other evidence-based approaches such as Acceptance and Commitment Therapy and Motivational Interviewing. We are able to select specific patient populations or disorders of interest in order to advance an intern’s training in a specific area or to address any gaps in training.
Pediatric and AYA (adolescent/young adult) Behavioral Medicine/ Psychology Clinic:
Supervisors: Jennifer Ludrosky, PhD; Stephany Lora, PsyD; Jonathan Perle, PhD, ABPP; Janelle Mentrikoski, PhD
Location: Chestnut Ridge Center
Interns will have the option to participate in fully integrated pediatric clinic(s), child/adolescent psychiatric consultation and liaison. Options include:
Pediatric GI Clinic: Interns will attend a half-day pediatric GI clinic (ages 0-18) in order to provide assessment, team consultation, and brief intervention for children and adolescents who present to Gastroenterology. Intervention areas frequently include anxiety, functional abdominal pain, adherence, adjustment to diagnosis, dietary change, encopresis.
Pediatric Nephrology Clinic: Interns will attend a half-day pediatric Nephrology clinic (ages 0-21) in order to provide assessment, team consultation, and brief intervention to children and adolescents who present to Nephrology. Intervention areas include adjustment to diagnosis, complex dietary change, adherence. Interns will practice using MI and stages of change with complex medical patients. Interns will also have the opportunity to join research projects, including examining the link between hypertension and anger in children, and the impact of COVID-19 on blood pressure in children and adolescents.
Pediatric Cleft Palate Clinic: Interns will attend a half-day pediatric Cleft Palate clinic (ages 0- 21) in order to provide psychology assessment and intervention to every clinic patient. Interns will become familiar with important concepts in the treatment of Cleft Lip and Palate and will work closely with large multidisciplinary team to provide high level care for children. Interns will also have the opportunity to gain skills in procedure management, as patients frequently have to undergo in-office procedures.
Attention Deficit/Behavior Clinic (AD/BC): Interns will attend a half-day pediatric clinic (ages 2-10) where they will learn to (1) provide diagnostic assessment of ADHD/disruptive behavior and comorbid challenges, as well as (2) how to implement parent management training strategies; one of the most effective evidence-based interventions for childhood disruptive behavior that is designed to improve compliance, on-task behavior, and parent-child relationships, while reducing problematic behaviors such as defiance and aggression.
Outpatient Pediatric Clinic: The intern will receive training in the provision of outpatient psychological treatment with children, adolescents, and parents. Cognitive Behavioral Therapy, play therapy techniques, and family systems and biopsychosocial theories will be utilized with patients with a variety of ages and presenting problems. Clinic can be focused on specific populations.
AYA (adolescent/young adult) Coping with Chronic Illness Clinic: The intern will participate in outpatient psychotherapy with adolescents and young adults who are living with a variety of chronic illness (e.g. diabetes). Interns will provide CBT focused therapy to help address issues common to this population, including treatment adherence, identity development, and transfer of care.
Supervisor: Stephanie Cox, PhD, ABPP; Laura Aylward, PhD
Location: Chestnut Ridge Center/ Department of Surgery
WVU Bariatrics offers a comprehensive surgical weight loss program including bariatric- trained surgeons, mid-level providers, dieticians, and psychologists. The intern has the opportunity to work as part of this multidisciplinary team in both assessment and intervention capacities. Interns receive training in pre-surgical psychological evaluations to determine a patient’s appropriateness for surgery. Additionally, interns can provide treatment to patients both pre and post surgically. Concerns commonly addressed include engagement in behavioral changes, treatment of disordered eating behavior, stabilization of psychiatric symptoms, etc. The intern also has the opportunity to attend team case review meetings and observe surgical procedures. The intern will also have the opportunity to lead and/or co-lead a monthly support group for pre- and postoperative patients.
Primary Care Behavioral Health
Supervisors: Barbara Cubic, PhD; Ruben Tinajero, PhD
Location: Clark K. Sleeth Family Medicine
The goal of this rotation is to increase the intern’s proficiency within the primary-care model; this includes the provision of population-based goal-oriented short-term treatment. The intern will participate in a variety of integrated primary care experiences including:
Integrated Outpatient Clinic:Behavioral health care is integrated into our primary care clinics within the patient-centered medical home model. Common presenting problems in this setting may include comorbid medical/ psychological concerns, insomnia, medication compliance, adjustment disorders, insomnia, relationship stressors, depression/ anxiety.
Family Medicine Inpatient Rounds/ Consultation: Family Medicine patients can continue to receive care by their primary care providers when they are admitted to Ruby Memorial Hospital. The intern has the opportunity to participate as a member of this multidisciplinary inpatient team (alongside residents, medical students, pharmacy, social work, etc.), providing consultation regarding psychological concerns and/or delivering brief psychological interventions in an inpatient setting.
Family Medicine Specialty Clinics: The Department of Family Medicine offers several clinics to provide patients with specialty care to address their specific need. These clinics include the Medical Weight Management Clinic, Diabetes Clinic, and COPD clinic (depending on availability/scheduling). The intern, as a member of these multidisciplinary teams, provides education and treatment of patients’ conditions, including management of psychosocial issues that often co-occur with chronic illnesses. The goal of this team approach is to improve patient outcomes and increase adherence to prescribed treatment regimens. The intern provides consultation and brief assessment or intervention as needed.