CCMD 701 Syllabus
2019 Syllabus
Problem-Based Learning
CCMD 701, Section 001
2 credits (facilitated small groups)
Course Description:
Students in this course work in facilitated groups to apply basic science concepts and principles to solve problems pertaining to clinical cases. Students are expected to develop and demonstrate independent learning and group communication skills. Students will also explore the roles of other health care practitioners, and learn to work in healthcare teams, through the use of inter-professional education exercises.
Expected Learning Outcomes:
Students in this course are expected to learn to:
- Integrate information across the various disciplines of basic and clinical sciences.
- Narrow the gap between basic and clinical sciences by using clinical cases to illustrate basic science principles.
- Enhance acquisition, retention and use of knowledge of the basic and clinical sciences.
- Enhance your self-directed learning skills
- Develop your communication and interpersonal skills working as part of a team
- Collaborate with learners in other professions
Specific Course Objectives:
Specific course objectives that will be assessed as evidence of achieving the learning outcomes relate to the six School of Medicine Core Competencies.
- Patient Care (PC)
- Medical Knowledge (MK)
- Practice-based Learning and Improvement (PBLI)
- Interpersonal and Communication Skills (ICS)
- Professionalism (PROF)
- Systems-based Practice (SBP)
Each of the six core competencies is further refined into a number of program learning objectives (PLOs). The competency area and PLO numbers are listed in parentheses for each course objective.
Students successfully completing this course will demonstrate ability to:
- Identify which organ systems, basic science disciplines, and social or cultural issues are relevant to each case presented. (PC2, PC3, MK1, MK3, SBP3)
- Define medical terminology, acronyms and abbreviations commonly used in a clinical context. (PC2, ICS5)
- Interpret physical exam findings, laboratory test results, and pathology reports to formulate hypotheses for a differential diagnosis of each case presented. (PC1, PC2, MK1, MK3, MK4, MK5, MK7, MK8, MK9)
- Collaborate with group members to rank hypotheses in order of probability of diagnosis based on evidence available, and revise hypotheses as new evidence is revealed. (PC2, MK3, MK4, MK7, MK9, PBLI5, ICS2, ICS4)
- Actively participate in group discussions of how each of the relevant basic sciences disciplines, including social and cultural issues, contributes to the signs, symptoms, and underlying causes of the conditions described in each case. (MK1, MK2, MK3, MK4, MK5, MK6, MK7, MK8, MK9, PBLI1, PBLI3, ICS2, ICS4, SBP3)
- Collaborate with group members to develop learning objectives that ask in-depth questions about basic science and social or cultural issues contributing to the cause or manifestations of disease or illness. (PC2, MK3, MK4, MK5, MK6, MK7, MK8, MK9, PBLI1, PLBI4, ICS2, ICS4, PROF3, SBP3)
- Independently research learning objectives for presentation to the group, including citation of primary sources utilized and use of appropriate methods to evaluate the reliability of sources for newly acquired information. (PC3, MK2, MK4, MK5, MK6, MK7, MK8, MK9, PBLI1, PBLI2, PBLI3, PBLI4, PBLI5, ICS2, ICS4, PROF5, SBP3)
- In collaboration with group members, integrate information across the basic and social sciences to develop a concept map for each case and use the mapping exercise to identify gaps in knowledge. (MK1, MK2, MK3, MK4, MK5, MK6, MK8, MK9, PBLI1, PBLI5, ICS2, ICS4)
- Rotate responsibilities for record-keeping, note-taking, reading case descriptions, and other tasks as applicable to individual cases. (PC1, ICS4, ICS5, PROF5)
- Arrive in class on time and prepared to present results of research into learning issues. (PROF5)
- Demonstrate respectful consideration of views of peers, and evaluate or critique concepts or ideas in a constructive manner. (PROF1, PROF5)
- Interact in a group setting with students representing other health-professions majors in order to define and practice roles in a health-care team, while developing improved interdisciplinary communication through inter-professional education exercises. (ICS2, ICS4, PROF1, SBP1)
Course Faculty:
The Problem-Based Learning course has three co-directors.
Heather Billings, Ph.D.
Department of Neurobiology & Anatomy
Room 4010C Health Sciences Center North
Phone: 304-293-1623
Steven Hardy, Ph.D.
Department of Physiology & Pharmacology
Room 3072A Health Sciences Center North
Phone: 304-293-1501
Andrew Shiemke, Ph.D.
Department of Biochemistry
Room 3103B Health Sciences Center North
Phone: 304-293-2310
In addition, students will be assigned to small groups, each with a faculty facilitator responsible for the group. Facilitators will be listed on the course SOLE site prior to the first day of class.
Course Schedule:
Group meetings to discuss cases are held on Wednesdays from 11:00 – 12:30 with your regularly assigned facilitator.
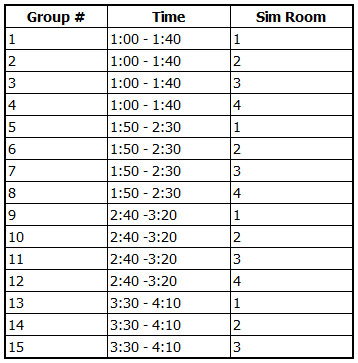
One case each term will involve one 40 min exercise in the simulation center, which will be scheduled based on simulation center availability and at a time that avoids conflict with other scheduled courses, including PDCI physician shadowing schedules. Day and time when each group should report to the simulation center will be announced by the first day of class and posted on the course SOLE site schedule.
Two 2-hour long inter-professional education (IPE) exercises will be held on Mondays from 4:00-6:00 PM. These sessions involve interactive exercises with students from the other health professions programs within the Health Sciences Center. The location where you should meet for this exercise will be posted on the SOLE site.
Sample schedule (exact dates to be determined annually as School of Medicine academic calendar is posted)
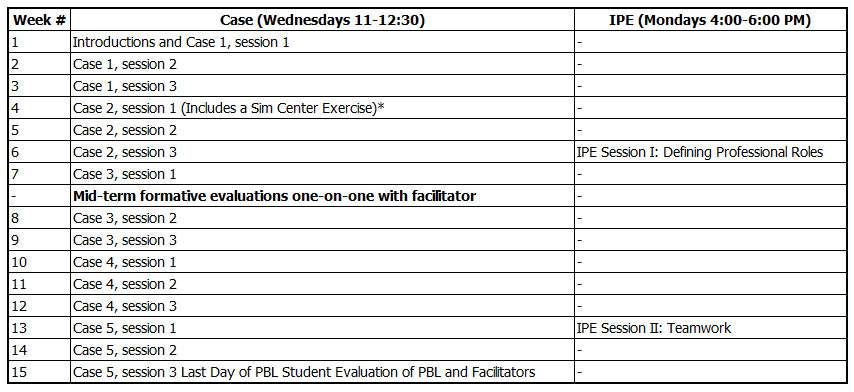
*The simulation center is reserved for PBL at the following times (date TBA):
Attendance Policy:
The success of PBL depends upon students working in a cohesive group, therefore, attendance is mandatory at all PBL sessions. Students are expected to arrive on time and remain until the end of the scheduled class period unless dismissed earlier by their facilitator. If you must miss a class due to illness or an emergency situation, contact your facilitator as soon as you are aware you will be unable to attend class.
Attendance and preparedness for class are covered under items 2. accountability, and 3. responsibility, within the School of Medicine Professionalism Code. Repeated absences or tardiness, and/or failure to notify your facilitator of an anticipated absence will be conveyed to the School of Medicine Committee for Academic and Professional Standards, and may result in disciplinary action.
Course Grading Policy:
Problem-Based Learning is a two-semester course. There will be a separate grade and narrative evaluation for each semester.
Formative Assessments:
Students will have multiple opportunities for formative assessments. PBL facilitators will encourage students to assess whether the PBL group members are participating and identify ways to maximize group collaboration periodically throughout the term. A mid-term one-on-one meeting with the group facilitator will also be conducted to help students identify weaknesses and concerns, and to develop a plan to ensure that all course objectives will be met prior to the final narrative assessment. The facilitators will submit a report on the student's mid-term progress to the course directors using eValue. Progress in each of the four areas of assessment will be included in this mid-term report. Students are encouraged to meet with their facilitators at additional times if they have concerns about course progress prior to or following the mid-term assessment.
Summative, Final Evaluation:
This course is graded on a Pass/Fail (P/F) basis.
In order to pass the PBL course, the student must demonstrate proficiency (Met or Exceeded Expectations) in all four areas of evaluation (described below). In addition, students will receive a narrative assessment, written by their facilitator that elaborates upon the students strengths and weaknesses.
There are four overall components that will be assessed, and students must demonstrate proficiency in all four categories (defined as met expectations or higher) to receive a passing grade in the course.
Areas of assessment for grading are as follows:
Demonstrates use of a knowledge base (assesses course objectives 1-3, 5):
- Integrates the three major perspectives of medical sciences (biological, behavioral, population) in cases and discussions.
Examples are:
• Defines major/relevant learning issues for each perspective.
• Gives examples from case of how one perspective might affect or interact with another.
• Develops management strategy to address the three perspectives. - Demonstrates understanding of issues across levels of organization (e.g., cellular and molecular; gross and microscopic; individual-family-community, organic and behavioral).
Examples are:
• Diagrams mechanisms using flow charts and other visual aids.
• Demonstrates understanding of key or rate-limiting steps. - Summarizes issues succinctly.
Examples are:
• Uses summary for clarification, checking understanding, integration, closure, or to set the stage for discussion.
• Presents case summaries that are concise and logical (i.e., have a beginning, middle, and end) and relates the learning issues/facts (i.e., the details) to the patient’s story (i.e., the big picture).
• Develops concise/specific learning issues by formulating questions that can be answered in the available time.
• Clarifies, focuses, and refines learning issues.
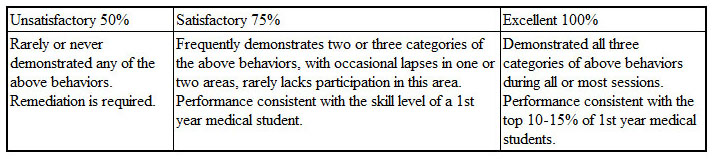
Grading Rubric:
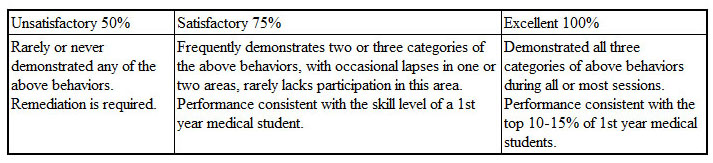
Demonstrates Knowledge Acquisition Skills (assesses course objectives 2, 3, 6, 7):
- Regularly develops learning issues.
Examples include:
• Asks key questions in showing inquisitiveness.
• Admits when knowledge is lacking.
• Identifies the ‘need to know’ in relating knowledge gaps to understanding the case at hand.
• Interacts with group to further define and ‘fine tune’ learning issues.
• Works to prioritize learning issues. - Presents learning issue research with proper depth and relevance, in a style that teaches well.
Examples include:
• Makes use of visual aids (black/white board, figures from books or Websites, overheads, etc.).
• Organizes information well before presenting it.
• Sorts research information to reflect the relevance of it to the case/Learning Issue at hand.
• Periodically during overall discussion adds information from own research that complements and supplements information presented by others.
• Brings unique/original resources to group. - Relates learning issues to the patient case or problem(s).
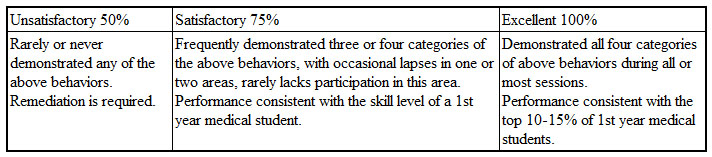
Grading Rubric:
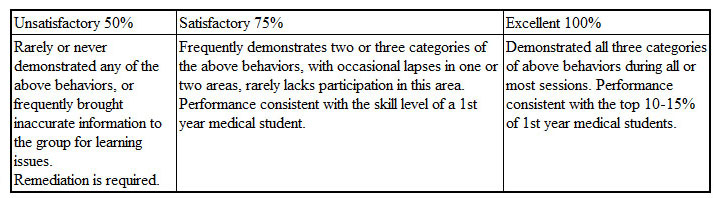
Demonstrates reasoning and problem solving skills (assesses course objectives 3, 4, 7, 8)
- Uses evidence to support reasoning.
Examples include:
• Supports reasoning and conclusions with relevant and specific information.
• Provides sources(s) of information cited. - Responds to uncertainty with a plan (e.g., identifies problem, formulates hypotheses, test hypotheses, and re-evaluates using written, personal, or electronic resources).
Examples include:
• Describes steps taken in seeking information.
• Selects resources that are relevant to group’s level of understanding.
• Able to choose from a variety of resources.
• Discerns relative value of resources used. - Uses reasoning process as part of the presentation/discussion of learning issues.
Examples include:
• Develops a plan and method for presenting learning issues that is understood by group.
• Conveys what is to be presented in a clear manner.
• Balances the level of detail to the needs of the group.
• Presents in a logical, step-wise manner (i.e., articulates start and end point of presentation).
• Reiterates and checks others’ understanding of learning issues.
Grading Rubric:
Demonstrates group communication and teamwork skills (assesses course objectives 5-12).
- Uses the board, diagrams, and audio-visual aids, including uses correct terminology and spelling, and writes legibly.
Examples include:
• Diagrams transferred to board are helpful.
• Spontaneously uses the board when necessary to graphically demonstrate difficult concepts with little or no prompting.
• Provides concise summary materials and uses them to facilitate group learning. - Uses active listening skills.
Examples include:
• Asks follow-up questions or clarifying questions.
• Reiterates or paraphrases to check understanding.
• Makes connections between information from different sources. - Uses verbal communication skills.
Examples include:
• Makes explicit the relationship of own and others’ contributions to previously discussed material.
• Explanations are clear and easily understood.
• Speaks clearly and succinctly, and with enthusiasm/interest. - Demonstrates team/helping behaviors.
Examples include:
• Checks others’ understanding, responds to lack of understanding in helpful manner, facilitating the learning of others.
• Facilitates the learning of others using questions which probe the level of understanding of conceptual material, as well as grasp of details and summarization.
• Challenges others’ concepts and ideas in a constructive way.
• Responds constructively to verbal and non-verbal communication in the group.
Grading Rubric:
Textbook:
There are no textbooks for this course.
Course materials will be distributed in each session by facilitators or electronically on the SOLE website.
Inclusivity Statement:
The West Virginia University community is committed to creating and fostering a positive learning and working environment based on open communication, mutual respect, and inclusion.
If you are a person with a disability and anticipate needing any type of accommodation in order to participate in this class, please advise me and make appropriate arrangements with the Office of Accessibility Services (293-6700). For more information on West Virginia University's Diversity, Equity, and Inclusion initiatives, please see http://diversity.wvu.edu.
Professionalism:
The West Virginia University School of Medicine strives to create a learning environment that furthers medical students' professional attributes. Our Code of Professionalism explicitly details the standard of appropriate behavior for all students, residents, faculty and staff. The nine primary areas of professional are defined as:
- honesty and integrity
- accountability
- responsibility
- respectful and nonjudgmental behavior
- compassion and empathy
- maturity
- skillful communication
- confidentiality and privacy in all patient affairs
- self-directed learning and appraisal skills.
Our Code of Professionalism can be found at:
https://medicine.hsc.wvu.edu/media/3006/code-of-professionalism.pdf
Personal dress, cleanliness, conduct and appearance are also important professionalism characteristics.
Our Professional Dress Policy can be found at:
https://medicine.hsc.wvu.edu/media/3008/guidelines-for-professional-dress.pdf
Student Code of Academic and Professional Integrity for the M.D. Degree Program
The West Virginia University School of Medicine requires students to adhere to rules of academic and professional integrity. The Student Code of Academic and Professional Integrity for the M.D. Degree Program details expectations of medical student behavior in lectures, examinations, laboratories, recitation sessions, clinics, all other academic settings. Successful progression through the curriculum and graduation with the M.D. degree are contingent upon the student's compliance with this code, which can be found at:
Mistreatment of Medical Students:
The West Virginia University School of Medicine defines and publicizes the standards of conduct for the faculty-student relationship and has a written policy for addressing violations of those standards. The Standards of Behavior for Interactions with Students (Dealing With Student Mistreatment) policy can be found at:
https://medicine.hsc.wvu.edu/media/3016/standards-of-behavior-for-interactions-with-students.pdf
Below is a summary of the key aspects of the policy:
- The medical school learning environment should facilitate mutual respect between teachers and students, staff and students, and between fellow students.
- While the perception of mistreatment may differ between individuals, examples of mistreatment may include:
Harassment of a sexual nature:
b. Discrimination based on age, race, gender, faith, national or ethnic origin, disability, sexual orientation, and veteran status;
c. Exclusion from any usual and reasonably expected educational opportunities for any reason other than the student’s performance;
d. Any physical or verbal misconduct inflicting bodily injury or emotional harm; and
e. Requirement to perform a menial task or tasks with the intent to humiliate. - If observed or the subject of mistreatment the student is required to report it to the campus Associate or Assistant Dean for Student Services. Students also have the ability to make anonymous reports of mistreatment using the E-value system. Directions to submit an anonymous report can be found in the WVU Medical Student Handbook on SOLE.
Other Policies and Procedures pertinent to the learning environment:
Grading Policy and Narrative Policy
https://sole.hsc.wvu.edu/Site/2843/Page?InstanceID=425938
Attendances and Absences during Inclement Weather
https://sole.hsc.wvu.edu/Site/2843/Page?InstanceID=426061
Policy for Appropriate Use of the Internet, Electronic Networking and Other Media